Medical Microbiology
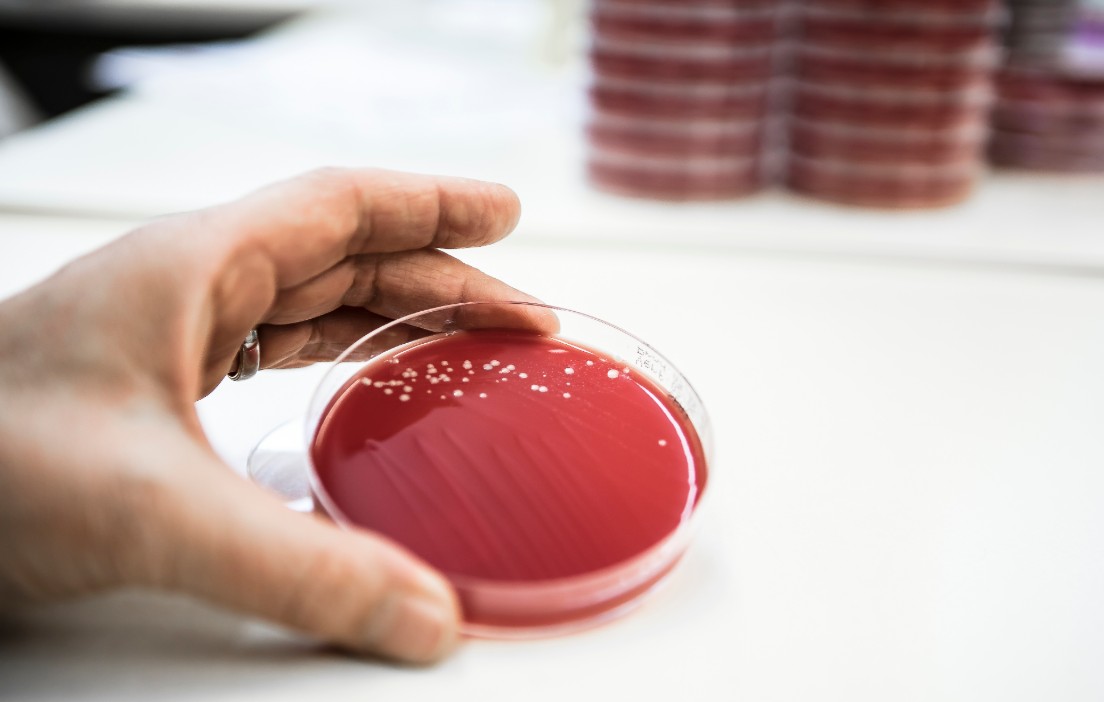
The Medical Microbiology department offers a comprehensive range of analyses pertaining to conventional and molecular bacteriology, mycology and parasitology. Our standardised work processes are based on recommendations issued by the American Society for Microbiology (ASM) and the European Society for Clinical Microbiology and Infectious Diseases (ESCMID), which ensures that all specimens are analysed consistently and to a high standard.
Fungi and parasite identification tests are performed daily, which also serves to boost our extensive experience. Our cooperation with the Molecular Diagnostics team allows us to identify even challenging and atypical isolates within a very short time with the help of 16S rDNA sequencing. Resistance testing is a key part of our work and is based on the latest EUCAST guidelines. We offer clinically relevant antibiograms for both inpatients and outpatients, which we supplement by also measuring minimum inhibitory concentrations (MICs) where necessary.
Range of analyses
Conventional, cultural bacteriology and mycology
- General bacteriology from a range of samples, including cerebrospinal fluid, tissue samples and punctures
- Mycoplasma/ureaplasma
- Detection of specific bacteria according to the indication, e.g. culture of Helicobacter pylori with resistance testing
- Fungi (yeasts and moulds, including dermatophytes)
Detection of antigens
- Clostridium difficile and toxin test (stool)
- Legionella pneumophila (urine)
- Streptococcus pneumoniae (urine)
- Rota- and adenovirus (stool)
Microscopy
- Ectoparasites
- Protozoa, helminths
- Urine and stool status
Pathogens detected by means of molecular biology
- Mycobacterium tuberculosis
- Urea- and mycoplasma
- Chlamydia
- Legionella
- Bordetella
Mycobacteria cultures and antibiograms are performed at the National Reference Center for Mycobacteria (NRC).
Resistance testing
The indication for resistance testing is based on the type and significance of an isolate. Whether resistance testing is possible from a technical perspective is primarily determined by the isolate. If the test can be performed, the result can be categorised as resistant (R), intermediate (I) or sensitive (S) if interpretation guidelines are available.
We categorise our results in line with the standards issued by the European Society of Clinical Microbiology and Infectious Diseases (ESCMID) and,
in individual cases, we refer to the American CLSI (Clinical Laboratory Standards Institute, previously known as NCCLS), information from literature or data provided by the antibiotics manufacturers.
The needs of both outpatients and inpatients were considered in the selection of the tested substances. In addition to the typical representatives of important substance groups for the detection of resistance phenotypes, oral antibiotics are preferred. EUCAST recommendations and the availability of the preparations on the Swiss market are further selection criteria.
Usful links
Swiss Society for Microbiology
ANRESIS (Swiss Centre for Antibiotic Resistance)
Swiss Society for Infectious Disease, Guidelines
Schweizerische Gesellschaft für Spitalhygiene, Richtlinien
Strategy Antibiotic resistance Switzerland (StAR)
Robert Koch Institut, Infectious Diseases
European Centre for Disease Prevention and Control
EUCAST European Committee on Antimicrobial Susceptibility Testing
Surveillance Atlas of Infectious Diseases
Your contact persons
DrVera Bruderer
Deputy Head Medical Microbiology
FAMH Microbiology

